News
AI Tool Promises Faster, More Accurate Cervical Cancer Treatment Planning
Published January 07, 2026
By Kimberly Mann Bruch, SDSC Communications

According to the World Health Organization, each year cervical cancer impacts approximately 600,000 women throughout the world and accounts for 340,000 global deaths. Brachytherapy is one of the best treatment methods for this type of cancer, but it is less frequently used because of the time required to design treatments for individual patients.
Researchers at the University of California San Diego have now developed a groundbreaking “one-click” AI tool that could transform how doctors plan these specialized radiation treatments for cervical cancer, saving physician time, reducing patient discomfort and minimizing the risk of human error.
Typically, personalized treatment plans for brachytherapy, a type of internal radiation therapy that targets a tumor while minimizing damage to healthy tissues, take an hour or more to develop, and rely heavily on the clinician’s skill. Sometimes, patients must wait under sedation while doctors fine-tune the plan. The process often varies between hospitals, leading to inconsistent treatment quality. New technologies developed by UC San Diego’s School of Computing, Information and Data Sciences researchers using the Voyager supercomputer at the San Diego Supercomputer Center (SDSC) can overcome these hurdles.
The new technology combines advanced deep learning with streamlined data processing. It was tested on hundreds of patient cases, and researchers found the tool’s plans matched the quality of those made by experienced doctors but took a fraction of the time.
“We used U.S. National Science Foundation NAIRR Pilot allocations on SDSC’s Voyager system to develop this new tool and built it into a widely used medical software platform so it’s easy for clinicians to utilize it,” explained Lance Moore, an AI researcher with the UC San Diego School of Medicine Department of Radiation Medicine and Applied Sciences. “The new tool uses AI to automate and speed up treatment planning and with just one click, the system analyzes a patient’s medical images and creates a high-quality, customized plan in less than four minutes — potentially reducing both the patient’s discomfort and the risk of human error.”
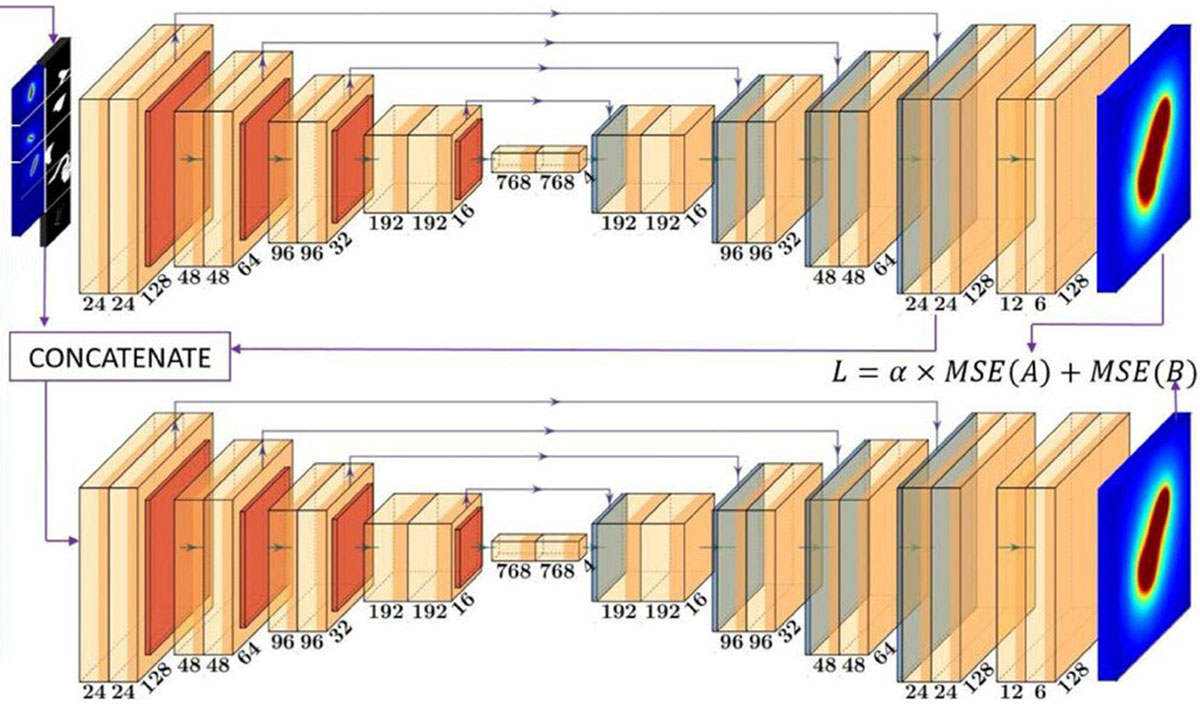
This two-stage AI model (called cascade U-Net) predicts the radiation dose for a brachytherapy plan. It takes simple images of the tumor, nearby organs and other planning images in order to make a patient-specific prediction. The first stage provides a rough estimate while the second stage refines the prediction. This approach allows the overall model to predict plans tailored to specific patients and their clinical needs. Credit: Lance Moore
Moore said that he worked with Paul Rodriguez, an SDSC computational data scientist, for initial setup, testing and benchmarking the model on the Voyager machine.
“This approach could help standardize care, especially in clinics with fewer resources or less specialized staff, and may allow more focus on improving plan quality rather than rushing to finish,” Moore said.
Looking forward, Moore said that the research team hopes to adapt their tool for other types of cancer, such as breast or prostate, and to make it easier to use in health systems everywhere. Ultimately, this AI advancement could deliver better, fairer cancer treatment to more patients, faster than ever before.
The work was published in the journal Brachytherapy.
Support for the use of Voyager was made possible by NSF NAIRR Pilot (allocation no. NAIRR250110). The Voyager system is funded by NSF (award no. 2005369).

